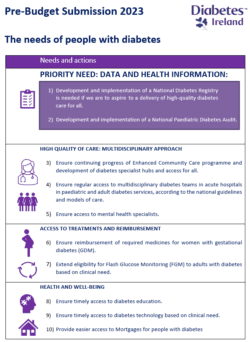
Diabetes Ireland presents its Pre-Budget 2023 submission to the Minister for Health and prioritise:
- the need to provide immediate funding for the development of a National Diabetes Registry and
- regular auditing of diabetes clinical services, so people with diabetes get access to similar standards of treatment and care regardless of where they live.
Diabetes Ireland presented its Pre-budget Submission 2023 to the Minister for Health Stephen Donnelly TD today and called on him and the Government to take a number of immediate actions to improve diabetes healthcare services for people with diabetes nationwide.
Diabetes is a serious global public health issue which has been described by the World Health Organisation as one of the top ten most challenging health problems in the 21st century with a high individual, social and economic burden. According to the International Diabetes Federation Diabetes Atlas 2021 Ireland is ranked 7th in the world for diabetes related health expenditure per person and in the Euro Diabetes Index 2014, Ireland was placed 20th out of 30 countries in the rank for the access to and quality of care and its outcomes One of the reasons for this low score was the lack of a diabetes registry, which helps to monitor the outcomes and supports health-services planning. Since 2014 nothing has changed in this matter and Ireland is still one of the very few countries in Europe which does not have a registry or routinely undertaken annual national audits of diabetes clinical services and diabetes outcomes. Both these issues need to be addressed as a priority in the coming budget.
Dr Kate Gajewska, Research and Advocacy Manager, Diabetes Ireland: If the HSE wants to aspire to deliver high-quality diabetes care, they need to know how many people live with diabetes in Ireland and where those people live. They also need to regularly monitor the standard of clinical care being provided along with diabetes outcomes. Only then can they begin to effectively plan staffing resources, determine the cost of providing care and improve health outcomes for our community.
There is no accurate figure available for the number of people living with diabetes in Ireland, but based on the Scottish prevalence data and the newest census, we estimate there are now approximately 300,000 people living with diabetes in Ireland. Furthermore, recent research has identified diabetes as the most prevalent chronic condition in people between 45 to 74 years of age in Ireland further implies the necessity of having access to appropriate data and health information so better decision making and planning can be undertaken.
Professor Hilary Hoey, Chairperson, Diabetes Ireland: In Ireland, some issues are the same for decades: these are over-stretched and under-resourced diabetes health services, in areas such as Cork, Donegal and Limerick. The lack of capacity and trained staff affects the HSE’s ability to meet the basic medical needs of people living with diabetes – it is responsible for very long waiting lists to access basic care, diabetes education or technology, which means access to regular and reliable diabetes care, high standards and modern treatments and medicines. An ongoing issue of significant under-resourcing is not acceptable.
To improve care in Ireland data provision is necessary and only then can appropriate interventions and decisions be made to address the multitude of issues. The entire diabetes community, including health care professionals, people living with diabetes, the HSE National Diabetes Clinical Programmes for Adults and Paediatrics and Diabetes Ireland agree that these priority needs are fundamental to generating positive change in how diabetes care is provided thus the priority ask of our Pre-Budget submission 2023 is to invest, develop and implement a National Diabetes Registry and a National Paediatric Diabetes Audit to be expanded into adult diabetes services eventually.
Diabetes Ireland has also highlighted a number of other issues in its submission including: the removal of the age restriction on the Flash Glucose Monitoring system, as Ireland is the only one Western European country with an age-restriction for this very well accepted glucose monitoring technology; the need to provide reimbursement of required medicines for women with gestational diabetes (GDM) to help protect both mother and baby, the need for extra staffing resources so people with Type 1 diabetes can get regular access to hospital diabetes services in line with national guidelines and HSE models of care. This would also improve access to timely diabetes education and diabetes technology based on clinical need.
The numbers of consultant endocrinologists, diabetes nurse specialists, dietitians and psychologists are low and the vast majority of clinics in Ireland are under-resourced. As outlined in the National Survey of Diabetes Care Delivery in Acute Hospitals 2018, ‘The current national WTE of consultant endocrinologists is estimated to be 72% lower than recommended minimum levels. Substantial staffing deficits were also identified across other disciplines with a national WTE percentage deficit of 95% in psychologists, a 74% deficit in dietitians, a 32% deficit in podiatrists and a 19% deficit in specialist diabetes nursing staff’.
Although the situation has slightly changed since 2018, in particular in dietetics, in nursing and psychology posts the deficits still exist and are still significant. These deficits were highlighted by the HSE National Clinical Programme for Diabetes in 2018, since then, however, staffing resources, local prevalence and needs have not been monitored or adequately addressed.
We are also concerned at the slow pace of development of the HSE Enhanced Community Care programme. Of particular concern is the employment of staff and the non-availability of appropriate accommodation for local services. We want assurances that the funding will be provided to employ the full quota of staff identified and that the service will be available free of charge upon GP referral for all people with diabetes who need it – not only to those who hold a GMS or GP Visit card. To avoid costly and unnecessary diabetes complications, investment must be made in best available diabetes care. There is much evidence that more frequent medical review reduces health costs by preventing acute and chronic complications and inpatient hospital admissions. Without this level of care for all people with diabetes, acute and chronic complications are increasing, thus, a reorganisation of the current delivery of diabetes care is warranted and the actions we are calling on the Government to support are person-centred, cost-effective, and easy to implement” Professor Hoey concluded.
Issued September 5th 2022
To read more about Diabetes Ireland Pre-budget Submission 2023 and how you can help, click here.